Thursday, December 24, 2009
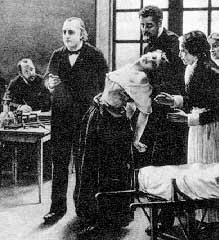
Morvan syndrome aka "Choree Fibrillaire"
Four cardinal features of Morvan syndrome are
1. Neuromyotonia or myokymia
2. Dysautonomia (esp hyperhidrosis, hypersalivation, labile hypertension). Weight loss is common.
3. Severe insomnia
4. Fluctuating encephalopathy with vivid hallucinations
Other notes-- MRI and random eeg is often normal. Patients are usually young males, EMG and PSG are not normal, and VGKC's are often present. Differential includes FFI, CJD, rabies virus, and Lewy body disease. The key clinical finding that differentiates is the dysautonomia and neuromyotonia. Often is fatal, but Ligouri et al. reversed one case with plasma exchange.
Ligouri R, Vincent A, Clover L, et al. Morvan's syndrome. Peripheral and central nervous system and cardiac involvement with antibodies to voltage gated potassium channels. Brain 124: 2417, 2001.
Note-- there is a second "Morvan's disease" that refers to atrophic changes in bone, skin, muscles of hand in syringomyelia.
Clinical spectrum of disease of VGKC
1. Autoimmune neuromyotonia (formerly Isaac's syndrome)
2. Morvan's syndrome (encephalopathy and myotonia). Augustus Morvan (1870) "la choree fibrillaire." see separate post on Morvan's in this blog
3. Encephalopathy without neuromuscular excitability--clinical syndrome consists of a) clinically indistinguishable from paraneoplastic limbic encephalitis (PLE) b) subacute cognitive impairment with behavioral changes and temporal lobe seizures c) FLAIR and T2 changes in mesial temporal lobes on MRI d) temporal lobe eeg abnormalities e) association with hyponatremia f) male predominance g) dramatic response to IVIG or steroids
4. Are occassional cases with associated cancer, especially lung and thymus carcinoma, but these are typically associated with "other" paraneoplastic markers and symptoms and are minority
5. A similar presentation and responsiveness to treatment occurs in VGKC negative patients who have anti hippocampal neuropil antibodies.
Monday, December 07, 2009
Coccidiodal meningitis and brain abscesses: analysis of 71 cases at a referral
Sunday, November 29, 2009
Idiopathic intracranial hypertension in men
Refsum like disorder in a Norwegian cosanguineous family
 -oxidation. We mapped the disease to a 15.96 Mb region on chromosome 20 (20p11.21-q12), containing approximately 200 genes (maximum lod score = 6.3).
-oxidation. We mapped the disease to a 15.96 Mb region on chromosome 20 (20p11.21-q12), containing approximately 200 genes (maximum lod score = 6.3). Saturday, November 28, 2009
Politics of health care reform in NEJM distort reality
The first article-- the best of the four-- describes how much FDA information never reaches clinicians (1). Clinicians and the public rely on the Food and Drug Administration (FDA) for drug and product approvals and denials, and for disseminating accurate information about drugs in their product inserts. I learned that the lengthy, often poorly written and weakly summarized debates about drugs are posted publicly at www.accessdata.fda.gov/scripts/cder/drugsatfda/. The authors cited glaring examples of critical information that somehow was not included in the product labels. Zometa (zoledronic acid, Novartis), used to treat hypercalcemia of malignancy, at the 8 mg dose, caused more renal toxicity and death than the 4 mg dose and was no more effective. Nonetheless, the labelling suggested using the higher dosage "in refractory cases." The product label did not mention increased mortality at the higher dose.
Lunesta (eszopiclone, Sepracor), sold 800 million dollars last year with the help of a direct to consumers marketing campaign. Yet the efficacy data, buried on page 306 of 403, shows patients slept 15 minutes earlier and 37 minutes longer than placebo, with no clinically meaningful improvement in next day alertness or functioning. Similarly, Rozerem (ramelteon), another approved sleep drug, caused younger adults to fall asleep 14 minutes earlier, and older ones 7 minutes earlier, with no improvement on subjective assessments of sleep quality.
The very next article details ways the same government can "further" improve health care. Victor Fuchs (2). advocates incremental rather than radical health care reform. The first of his four proposed reforms is to eliminate employer based health care coverage tax exemptions. The purpose is to raise 200 billion dollars in new revenues, that is taxes, to make the tax system "fairer" since the tax benefit is a regressive tax. He alleges it benefits the wealthy. (Wait a minute-- my practice employs 15 people, who have relatively low incomes and have the same insurance I have. A biller who had breast cancer last year would never have gotten treatment without our comprehensive health insurance). This would allow the creation of insurance exchanges, the second idea, that would, using Fuchs' words, be not as "generous" to "consumers" (actually, sick patients) as the private plans they replace. Supposedly, these exchanges would decrease "broker" costs.
The third, chilling suggestion of Fuchs is the appointment of an "expert" commission to devise changes to the ways Medicare reimburses providers. Fuchs cites "special interests" as blocking the "public good," as a charged way to rally the troops. Again, citing my own practice, with 50 % overhead, a 10 % payment cut equals a 20 % loss of income. Could it be, that by going after providers who have already been sucked dry, Fuchs will drive people out of practice, resulting in fewer providers, thereby raising the cost of care? Fuchs' final idea is an office for technology assessment that would be "quasi-independent." Of whom, I might ask.
The third article-- the last to be reviewed here- describes implementing evidence based medicine in Washington state (3). The state has total authority, except where prohibited by federal statute, to use evidence based methods to assess drugs, devices, surgical procedures, diagnostic tests, imaging procedures, and medical equipment. The author decries the political "pressure" wrought by patients who testify that the benefitted from a technology the state wants to eliminate. Obscenely, the same authors equate pharmaceutical direct to patient marketing with physician "autonomy" and "financial incentive" in ordering tests.
The authors note the "challenges" of this policy, citing the example that thymectomy of myasthenia gravis, used since 1912, has never undergone a rigorous trial. This author will note a few more nonevidence based treatments: penicillin for infection, appendectomy for appendicitis, and burr holes for subdural hematomas of the brain. Are these procedures necessary? Shall the government be in a position to decide? May I be so impudent to suggest satisfaction surveys be returned for all cases of physician assisted suicide?
The assumption of evidence based medicine is that care from one can be generalized to another and is equivalent to another. Evidence is important, and can help us learn how to be better doctors. But, evidence is not the be all and end all. Sometimes doctors have to take the controls from the nurse practitioners and PhD's and make decisions that are in the best interests of the patient. The reasons may not be obvious to the lay public but may be based on sound understanding of pathophysiology. Experience and judgment, absent from these vacuous bureaucratic declarations, still are what most patients seek.
1. Schwartz LM, Woloshin S. Lost in transmission: FDA drug information that never reaches clinicians. N Engl J Med 2009; 361:1717-1720.
2. Fuchs VR. Four health care reforms for 2009. N Engl. J Med 2009; 361: 1720-1722.
3. Franklin GM, Budenholzer BR. Implementing evidence based health policy in Washington State. N Engl J Med 2009; 361:1722-1725.
Friday, November 27, 2009
Idiopathic recurring stupor & narcolepsy automatisms
Several sleep related conditions may mimic and be misdiagnosed as seizures. 80 % of narcoleptics have automatic behavior during sleep. The individual appears awake but is without full awareness. Behavior may be inappropriate and resemble a fugue state.
Idiopathic recurring stupor was described in 1990. The stupors may occur a few times weekly to a few times annually, and last from hours to days. All cases show a widely distributed nonreactive 13-18 hz activity. Flumazeni, a benzodiazepine antagonist, quickly but temporariy reverses the stupor and eeg findings. The culprit is thought to be endogenous benzodiazepines called "enzopines" that act on the GABA A receptor for benzodiazepines. These ligands may alsobe important in learning, memory, hepatic encephalopathy, and panic attacks. CSF enxopine-4 levels are more than 100x higher than in control subjects.
Thursday, November 26, 2009
The Larynx for Neurologists
Meyer TK. The Neurologist 2009; 15:313-318. Also points from Rosenfield DB,and Viswanath NS. Neurolaryngology.in Evans R. Diagnostic Testing in Neurology Philadelpia, Saunders, 1999, pp. 223-229.
Larynx functions: phonation, deglutition, airway protection, control of respiration. Laryngeal closure also allows increased abdominal pressure for defection, parturition and stabilization of thorax for heavy lifting.Humans have a lower larynx than grazing animals,helping phonation but more precarious for airway control.
Diseases
Parkinson's disease-- vocal folds are atrophied and bowed with incomplete closure. Patients perceive their own hypophonic speech as of adequate loudness. Voice is also due to bradykinetic efforts from inadequate bellows mechanism (diaphragm and chest wall). Treatment includes bilateral bulking injections to vocal cords to facilitate glottal closure which can be temporary or permanent. Lee Silverman voice technique also helps.
Vocal Cord paralysis. Patient has weak breathy wet voice. It usually occurs due to tumor or surgery. If one vocal cord does not close, can do implant medialization, which will improve voicing and cough in all, and speech in 70 %.
Spasmodic dysphonia-- is a focal dystonia of 2 types. Adductor s.d. is characerized by harsh strangled quality with voice breaks. Abductor s.d is characterized by sustained breathiness with breathy voice breaks. The dystonia is task specific, eg. with breathing, sparing other functions such as swallowing. SD is female predominant with 73 % ADSD, 17% ABSD. Its associated with essential tremor in 30 % and other dystonias in 14 %. Botox is best treatmentfor both types, although the procedure is different for each.
Historical points in dysphonia. Getting stuck,shaking, or improving with alcoholsuggests ET. Trauma can cause dislocated arytenoid cartilage. Pain indicates focal pathology or GERD. Abrupt onset maybe psychogenic. Fluctuations may represent myasthenia.
Signs--
some physical exam tests for conversion disorder
2 Hysterical dysphonia. The vocal cords are normal during larygoscopy, cough is normal, articulation in whisper is normal.
3. Monrad Krohn's cough test for hysterical monoparesis. Stands behind patient, grab both lattismus dorsi,ask patient to cough, lats contract prove integrity of brachial plexus.
4. Double crossed arm pull test for hysterical monoparesis. Grab patient's wrists which are crossed across his chest and tell him, "when I say now, pull back as hard as you can." He may pull both sides.
5. "Make a fist " test for psychogenic wrist drop. Wrist elevates with a fist (functional position) or with holding a pencil in posiition.
6. Reversed hands test for functional monoparesis. Interlock hands, ask patient to move finger pointed to.
7. Backward displacement test for psychogenic foot drop. Push patient backwards and see anterior tib dorsiflexors spring into action.
8. Hoover test.One hand under each heel. Ask patient to raise the good leg, and the other one will inadvertently push down in functional patient. If ask patient to push down with both legs, if organically paralyzed he won't if hysterical he might.
9.Raimiste's leg abduction/adduction test for hysterical weakness. Similar to Hoover test for abduction and adduction of legs.
10. Psychogenic visual field deficit with tubular vision, same deficit for near and far Similar, spiral visual field defect may occur with smalllr field with each trial.
Provocative sensory tests pearls
2. Pallanesthesia refers to vibratory testing.
3. The directional scratch test on the dorsum of the palm and leg may be superior to other tests of vibratory or position sense (Hankey and Edis, JNNP, 1989). Scratch a line across 2 cm and ask patient if scratch was up or down. If unable to perform accurately (ie, 100 %), repeat with distance systematically increased to make the test quantitative.
4. Two point discrimation with a paper clip can be done touching the patient with one or both ends of the paper clip and asking if patient got one or more than touch. Thresholds for normal two point discrimination in patients more than 7 years old, 2-4 mm on fingertips, 4-6 mm on dorsum of fingers, 8-12 mm on palms, 20-30 mm on dorsum of hands,
Wednesday, November 25, 2009
Circadian rhythm disorders-- P Zee
1. Keeping time can be regulated at a genetic molecular level with clock genes. This affects both ASPD and DSPD.
2. SCN sends a signal to pineal, which feedbacks to SCN altering circadian rhythms. The main influences on are light, melatonin, and physical activity.
3. Advanced or delayed circadian rhythm disorders occur. Assess with: 7 day eveningness/morningness questionnnaire, sleep diary, actigraphy, core body temperature, melatonin level (24 hour or sleep onset DLMO, clinically available, from saliva) or PSG- ambulatory .
4. Advanced and delayed sleep phase disorder. Rectal body temp usually nadirs 4-6 am, so someone who nadirs at 11 am (college kid?) has a delayed circ disorder. Same patient, melatonin spikes at 1 am whereas for most of us it happens at 9 pm. DSPS has higher rate of BPAD
jet lag pier.acponline.org googlejetlag calculator
east ward trouble falling asleep
west ward trouble staying asleep.
if lags going to Europe, avoid bright light in AM. Speeds up realignment.Needs a week to realign otherwise. Going back west, use melatonin at bedtime at destination.
Other quick hits
REM sleep centers include pons -- perilocus cereleus for atonia, and vestibular nuclei for generation of REM and basal forebrain also plays a role as do other areas.
Sleep pearls, neuromuscular diseases other than ALS
Pearls on sleep disorders in ALS
Pearls on melatonin and sleep timing Moore
Wednesday, November 18, 2009
Presentations of adult onset leukodystrophy
Costello DJ et al. The Neurologist 2009;15:319-328
ALD kids get spastic paraparesis with detrusor instability. Defect is VLFA's ABCD1 mutation. MRI lesion is leukodystrophy starting posteriorly, may enhance partially and be confused with inflammatory disease. Adults may present with neuropsychiatric disease, followed by spasticity, ataxia, seizures, and death. Two thirds of female carriers also develop some sort of progressive myelopathic picture. They may have more pain and be misdiagnosed as having MS or fibromyalgia. Adult cerebral (AC-ALD) is more fulminant than X-ALD.
MLD is aut rec. Presentations in younger patients include disturbed gait, ataxia, quadriplegia, optic atrophy, and peripheral neuropathy, to decerebrate rigidity. In adults, presentation is often neuropsychiatric with misdiagnosis of schizophrenia, or even normal, with neuropscyh testing especially showing problems with visuospatial construction. There are dramatic elevated sulfatides due to arylsulfatase deficiency.
In Krabbe disease, beta galactocerberosidase occurs, is characterized by , in adult form, various motor presentations with progressive cognitive decline, seizures, cortical blindness with 20 % having uniform slowing of nerve conduction studies. Substrate (galactosylceramide) levels are increased but only mildly, but within oligodendrocyte, there are 100 fold increases in psychosine which is cytotoxic and selectively damages oligodendrocytes. Its been described up to age 84. Get posterior predominant involvement, no enhancement.
In Vanishing White matter disease, adult onset, there is cognitive involvement, pseudobulbar palsy, spastic paraparesis, with an important association with ovarian failure, "ovarioleukodystrophy." Its caused by mutations in e1f2b, affects ribosomes and proteins, causes cystic degeneration and rarefaction of the white matter. Clinical features not completely understood, probably is more common than thought.
Alexander disease-- due to mutation in GFAP, causes Rosenthal fibers. Get bulbar and pseudobulbar palsy with white matter abnormalities starting in front.
Canavan disease-- increased NAA in urine, Spectroscopy is good to diagnose this.
Hereditary diffuse leukoencephalopathy with spheroids is almost exclusively diagnosed in adults. Present with deteriorated behavior and personality and seizures. Diagnosis is by tissue.
Pelizaeus Merzbacher is X linked but like ALD carrier females have a forme of disease. Tremor, ataxia, dementia, and progressive spastic paraplegia occur. Mutation on PLP 1 on X q 22 occur. Classic hypomyelinated CNS disorder.
Recessive hypomyelinating leukoencephalopathy (RHL) =PM like disease is a hypomyelinating disease.
others see text, also for Rx
Emerging neuro infections: CHIK, Hendra & Nipah viruses
CHIK virus
infection due to enhanced vector competence. Spread by mosquitoes to humans, togavirus. Abrupt onset fever, joint swelling, myalgia, headache, back pain, and rash. Diagnosis is by CDC IgM and IgG. Rare neurologic cases include encephalitic infections of newborns and elderly.
Other presentations include encephalomyelitis, myeloradiculitis, acute flaccid paralysis (GBS like), encephalopathy and seizures. A mutation in viral envelope dramatically changed infectivity. Endemic travellers to new areas cause infections
Nipah and Hendra viruses.
classification is henipavirus of paramyxovirus. In Australia it first was identified as a highly infectious disease of horses and close human contacts/handlers. Aseptic meningitis and encephalitis occurred in Hendra, a location in Australia.
Nipah virus, closely related, occurred in pig farms in Singapore and Malaysia in 1998. Encephalitis and pneumonitis were common, with a 40 % mortality. The incubation perido was two weeks, with a 3-4 day prodrome. Mortality was 73 %. MRI usually showed multiple small subcortical lesions on T2 and FLAIR images without edema. PEARL- relapsing and delayed onset disease can occur. in 3 % or so average 8 months after first event, with an acute onset the second time. There was an associated systemic vasculitis with thrombosis and parenchymal necrosis in the CNS. Syncytial multinucleated endothelial cells are pathognomomic and occurred in 25 %. A subsequent outbreak in Bangladesh was not associated with pig farms and was shown to be associated with flying foxes and fruit bats with spread through urine of latter. Human to human transmission occurred, including between patients and health care workers.
Monkeypox virus causing neurologic human infection
Tyler KL. Emerging viral infections of the CNS. Part II. Arch Neurol 2009; 66: 1065-74.
Due to exotic pet (mammal ) trade from Africa including Gambian pouched rats, dormouse, and rope squirrels, spread to prairie dogs in the US to humans.
Most common symptoms, 50 percent or more have rash, fever, chills, adenopathy, myalgias, sweats and cough. Rash follows several days later and typically is maculopapular, proceeding through stages with papules, vesicles, and pustules. The rash is centifugal and involves the hands or feet in 80 %, legs or feet in 65 %, head in 6 %, and resembles chicken pox. Unlike chicken pox (and like syphilis and ricketsial infection) there is lymphadenopathy and involvement of the palms of the hands and soles of the feet. Diagnosis is with skin biopsy, PCR, and ELISA.
One six year old developed encephalitis. Diagnosis was made by serum IgM and IgG and CSF IgM, with negative PCR.
Sunday, November 15, 2009
rituxan and MG details
Rituximab for myasthenia gravis developing after bone marrow transplant
Lebrun C, Bourg V, Tieulie N, et al. Successful treatment of refractory generalized myasthenia gravis with Rituximab. Eur J Neurol 2009: 16: 246-250. 6 patients with refractory disease after thymectomy , got 375 mg/m2 weekly for four weeks then monthly for for two months, then subsequently based on clinical status. A few patients needed infusions for 1-2 years. All patients ultimately tapered mestinon and prednisone and other drugs.
Diaz-Manera J, Martinez Hernandez E, Querol L. et al. Long lasting treatment effect of rituximab in MuSK myasthenia. Neurology 2012; 78: 189-193 . 17 patients with resistant MG 9defined as failing 3 second line agents. Rituxan was given 375 mg/m2 for four weeks then monthly for two months, then if intereference with ADL's. All patients with uSK reached minimal manifestation status by 3 months after treatment, and maintained MMS or remitted by 35 months. Note-- drug seems best suited for MuSK patients.
Anderson et al.Rituxan in refractory myasthenia gravis: a prospective open-label study with long term followup.. Ann Clin Trans Neurol 2016; 3: 552-555. Refractory MG given Rituxan by abvove protocol or 750 mg/m2 every 2 weeks x 1 month. 3 people got additional cycles. At 22 months all patients improved, and pred, IVIG and PE needs decreased.
One case exists of PML in a MuSK myasthenic patient (Kanth KM, Solórzano GE, Goldman MD. PML in a patient with myasthenia gravis treated with multiple immunosuppressing agents. Neurol Clin Prac. 2016; 6: e17-e19).
Durability of responseRobeson KR, Kumar A, Keung B et al. Durability of the rituximab response in acetylcholine receptor autoantibodfy positive myasthenia gravis. JAMA Neurol 2016 : 4190.
After the first cycle, 63 % had sustained remission, 19 % had pharmacological remission and 19 % MMS not requiring treatment.
Of those who discontinued all other forms of therapy, did so at a mean of 8 months (range 1-13) after the last cycle. 9/16 (56 %) relapsed at aa mean of 36 months, but all improved with further immunosuppressive therapy. All patietns tolerated it well.
+ four more.
Annot. bibliography B cell function, myasthenia
Zebardast N, Patwa HS, Novella SP, Goldstein JM. Rituximab in the management of refractory myasthenia gravis Muscle Nerve. 2009 Oct 22. (Yale). Studied six refractory patients. Began rituxan 375 mg/m2 weekly for 6 weeks, then 2 treatments every 20-30 days and decreased prednisone. 8 months later received a second course of 5 infusions weekly. A third course of 4 weekly infusions were given 6 months after that. All patients received 4-6 doses of weekly infusion, with subsequent infusions at 6 months if needed.
Nelson RP Jr, Pascuzzi RM, Kessler K, Walsh LE, Faught PP, Ramanuja S, Pescovitz MD, Loehrer PJ Sr. Rituximab for the treatment of thymoma-associated and de novo myasthenia gravis: 3 cases and review. J Clin Neuromuscul Dis. 2009 Jun;10(4):170-7. Review.
Stieglbauer K, Topakian R, Schäffer V, Aichner FT. Rituximab for myasthenia gravis: three case reports and review of the literature.J Neurol Sci. 2009 May 15;280(1-2):120-2. Epub 2009 Mar 9. Review.
Lebrun C, Bourg V, Tieulie N, Thomas P. Successful treatment of refractory generalized myasthenia gravis with rituximab.Eur J Neurol. 2009 Feb;16(2):246-50. Authors followed 6 patients with poor response to immunosuppressive meds. All but one were ACH receptor negative and 3 were anti Musk positive. IVIG did not help. Doses: 375 mg/m2 weekly for 4 weeks After one month steroids were discontinued and anticholinesterase meds decreased. Rituxan cont. every 2 months for six months. Benefit persisted for 2 years of f/u (patient one). Steroids were tapered after the first infusion.
Stübgen JP. B cell-targeted therapy with rituximab and autoimmune neuromuscular disorders. J Neuroimmunol. 2008 Nov 15;204(1-2):1-12. Review.
Illa I, Diaz-Manera J, Rojas-Garcia R, Pradas J, Rey A, Blesa R, Juarez C, Gallardo E.Sustained response to Rituximab in anti-AChR and anti-MuSK positive Myasthenia Gravis patients.J Neuroimmunol. 2008 Sep 15;201-202:90-4. Epub 2008 Jul 23.
Dalakas MC.Invited article: inhibition of B cell functions: implications for neurology.Neurology. 2008 Jun 3;70(23):2252-60. Review.
Saturday, November 14, 2009
Pearls on AIDS related neuropathies
1. Antiretroviral distal sensory neuropathy (ARV-DSP) occurs with didanosin (ddI), zalcitarabine (ddC), stavudine (d4T) plus more recently, adanavir, saquinavir, and ritonavir. It occurs chiefly in first year of treatment or in patients with preexisting neuropathy. Symptoms occur with drug onset and resolve with discontinuation of the drug.
2. DSP due to HIV was formerly associated with high viral load, and low CD4 count and occurs in nearly 100 % at autopsy, and 30-50 percent in clinical practice. Other risk factors are older age, low nadir CD4 count, poor nutrition, coexisting diabetes, and use of neurotoxic drugs (such as antiretrovirals) or alcohol.
3. Of newer drugs, duloxetine is FDA approved for DPNP (diabetic peripheral neuropathy pain) and is under study in HIV DSP. Lamotrigine has been shown to be effective. Elavil and NSIAAD's have not been shown to work.
4. Polyradiculitis is usually pure motor and can be due to CMV, TB, cryptoccosis, and meningeal lymphocytosis. Treponema also has been described. Presentation was usually progressive weakness starting weeks before onset. One case had cervical disease, the rest were lumbar.
Tuesday, November 10, 2009
Hardscience of concussions
rapid acceleration and deceleration of brain can be estimated as follows
a=(v2-v0)/2sg, easily calculates deceleration based on initial speed v0, final speed v2, and distance travelled s. The result obtained is in terms of g, which is equivalent to 10.73 yards per second (Varney and Roberts 1999). Since the final speed is zero after player stops, formula becomes a= -v0squared/2sg. Then, calculate force applies by F=mg. The number 200g force has been proposed as the amount to cause permanent damage but is not really known.
Brain injury in organized sports
Mendez MF. The neuropsychiatric aspects of boxing. Int J Neuropsychiatry Med 25: 249-262, 1995.
Stewart WF, Gordon B, Selnes O. et al. Prospective study of central nervous system function in amateur boxers in the United States. Am. J Epidem 139;573-588, 1994. Bouts fought before 1984 when safety measures were instituted were correlated with neuropsychological impairments.
Football
Abnormalities in sustained attention and visuomotor speed with absent normal practice effects. Preseason baseline assessment by SLAM model is becoming gold standard for concussion assessment and management.
Sideline assessment use SAC,a 5-10 minite measure (McCrea et al, 1996).
Mild traumatic brain injury important articles
JT Barth et al, 1989, 2002 4 yr prospective study of MTBI in college athletics in Sports Laboratory Assessment model (SLAM) with 2300 football players at 10 universities with pre and post neuropsychological assessments. It used a matched control group plus patients as their own control group. After very mild injuries athletes showed a 5-10 day recovery curve for mild cognitive deficits.
Consensus Conference: Rehabilitation of persons with traumatic brain injury . NIH Consensus Development Panel on Rehabilitation of Persons with TBI. JAMA 282:974-983, 1999. Neuropsychological deficits include problems with memory, attention, concentration, executive skills.
Thursday, October 22, 2009
Wednesday, October 14, 2009
Adult onset ataxia telangiectasia (variant AT)
Monday, October 12, 2009
MGUS: significant beyond hematology
Vanderschueren SW, Mylle M, Dierickx D et al. Monoclonal gammopathy of undetermined significance: significant beyong hematology. Mayo Clin Proc. 2009; 84:842-847.
MGUS is found in 3% of patients older than 50, 5% older than 70, in 7 % of patients seeking medical evaluation, and converts to myeloma at rate of one percent per year. Authors present five OTHER associations of MGUS that are commonly underrecognized.
1. Acquired C1 inhibitor deficiency. should be suspected in patients with repetitive often stereotypic episodes of angioedema, with no urticaria or pruritus or family history, & in pts with recurrent acute abdomen with normal CRP and low C4 levels. Hereditary form occurs in first two decades usually, acquired forms in elderly patients with MGUS in up to 40 % of cases (IgG, IgM or IgA). In acquired forms C1q levels are low due to consumption. Acute prophylaxis can be done with antifibrinolytics eg. transexamic acid or danazol, and acutely FFP has variable success.
2. Systemic capillary leak syndrome should be suspected in patients with repetitive hypovolemic shock, capillary leak and hemoconcentration (in case report, HB went from 15 to 23 in one day). Attacks characterized by prodrome malaise, fatigue, OH, polydipsia, palpebral edema, last 1 to several days and have high fluid requirements during an attack. MGUS usually IgG is typically present. Intestinal edema, ascites, muscular edema, pleural and pericardia effusions occur, may have compartment syndrome. Terbutaline, theophylline, and IVIG are used to treat.
3. Acquired von Willebrand syndrome-- uncommon condition occurs in elderly patietns with no history or family history of bleeding, with MGUS in 50-60 %. Desmopressin works transiently. High dose IVIG has been used. Suspect with mucocutaneous or postop bleeding.
4. Schnitzler syndrome-- heralded by repetitive fevers and chronic, initially nonpruritic urticaria. CRP and ESR are typically very high. MGUS is usually M type. Anakinra, an IL1 antagonist shows promise.
5. Scleromyxedema-- characterized by typical skin eruption and visceral or repetitive neurologic involvement. Case reported of 39 yo man with episodic confusion preceded by flu like illness proceeding to status epilepticus and prolonged postictal coma. Over weeks, appeared erythematous plaques on face and skin creases over glabella , confirmed with biopsy to be scleromyxedema. Tx was plasmapx, IVIG, dexamethasone, autologous stem cell, thalidomide. Its caused by hyaluronic acid deposition in superficial dermis and production of MGUS usually IgA. Also called papular mucinosis and generalized lichen myxedematosus. Occurs in patients usually 30-50 , may include MI as well. Also called dermatoneural syndrome.
Monday, September 28, 2009
Neuroopthalmology of chiasm: Pearls
1. a prefixed chiasm can result in deficit resembling congruous visual field loss
2. A postfixed chiasm can resemble bilateral optic neuropathy
3. Fixation blindness: attempts to focus on a near target results in overlap of 2 nonseeing temporal fields, and everything beyond fixation appears to disappear.
4. See saw nystagmus seen with masses or trauma cause one eye and other alternately elevating, intorting, and then depressing and extorting, in a pendular fashion
5. Gliomas of chiasm are similar to optic nerves, presenting with decreased vision, optic atrophy and strabismus
6. In pituitary apoplexy, pain is frequently retroorbital, and field defect is classically bitemporal superior quadrantanopsias, due to upward expansion of the tumor, 70 % vomit, LP is abnormal, MRI is diagnostic test of choice, and substantial medicolegal risk resides therein. Men have nmore than women
7. Aneurysms causing chiasmal compression include supraclinoid ICA, the ICA-opthalm a junction, and occassionally cavernous or ACOM arteries. Nonruptured aneurysms causing compression require treatment usually with clipping rather than coiling (Continuum 2009).
Compressive optic neuropathies- dDx
primary tumors
glioma
ganglioglioma
capillary/cavernous hemangioma
melanocytoma
secondary tumors
metastatic carcinoma
nasopharyngeal carcinoma
leukemia
lymphoma
infectious/inflammatory
sarcoidosis
lupus
APL syndrome
paraneoplastic syndrome
Wegener's granulomatosis
GCA
PAN
IBD
Behcet's
Sjogren's
postvaccination
perioptic neuritis
Infectious (TB, syphilis, lyme)
Viral (HSV, HIV, CMV, EBV, Cox A, Hep A, Hep B, MMR, rubeola)
fungi (aspergillus, mucor, crypto, candida, histoplasmosis
parasites ( toxo, cysticercosis, toxicariasis)
Sarcoid and lupus related eye diseases
-- Anterior uveitis (most common)
--optic neuritis like
--Perineuritis
--retrobulbar optic neuropathy
-- granulomatous infiltration of the posterior orbital, intracanalicular, and intracranial optic nn.
All have disc edema (eventually)
May have slowly progressive or acute vision loss
diagnosis may be helped by findings of conjunctival nodules, uveitis, lacrimal gland enlargement, and vitreous opacities.
lupus
--PION more common, but AION occurs
-- can see IIH like presentation (except not really "idiopathic"
Thursday, September 24, 2009
Intranasal contact point headache
Rozen TD. In...: missing the point on brain MRI. Neuroimages. Neurology 2009; 1107.
Nasal septal deviation with contact point on the lateral naasal wall can trigger episodic or daily headaches. Its easy to visualize on MRI but rarely reported. Authors show an image of an MRI of 2 cases.
REM Behavior Disorder (RBD) Random Pearls
2. Differential diagnosis would include OSA which causes disruptions in sleep architecture and increased nighttime arousals so sleep study for that problem would be useful (pseudoRBD)
3. Drugs that cause/exacerbate include SSRI's, TCA's, MAO A inh, ETOH withdrawal,
4. Actions can be purposeful violence as patients are actually enacting dreams which are violent
5. Dreams of being chased are common (50 v. 8 % in RBD v. non RBD PD patients)
6. Associated with synucleinopathies ie. PD, CBD, LBD (52 % risk at 12 years)
7. Environmental precautions are medicolegally important including separate beds, locking windows, etc.
8. Effectively treated in 90 % with clonazepam, with most of the rest treated with carbamazepine.
9. Patients can have nonviolent behaviors as well as violent ones including included masturbating-like behavior and coitus-like pelvic thrusting, mimicking eating and drinking, urinating and defecating, displaying pleasant behaviors (laughing, singing, dancing, whistling, smoking a fictive cigarette, clapping and gesturing "thumbs up"), greeting, flying, building a stair, dealing textiles, inspecting the army, searching a treasure, and giving lessons. Speeches were mumbled or contained logical sentences with normal prosody. In PD with RBD (n = 60), 18% of patients displayed nonviolent behaviors. In this series (but not in incidental cases), all RBD patients with nonviolent behaviors also showed violent behaviors. NEUROLOGY 2009;72:551-557
Wednesday, September 23, 2009
Orthostatic tremor; writing tremor
ET v PD
Coat hanger sign of orthostatic hypotension and other MSA pearls/ signs
Tuesday, September 22, 2009
red flags for psychogenic movement disorders
psychogenic dystonia
Psychogenic Parkinson's clues
psychogenic movement disorders features
Saturday, August 15, 2009
Drugs that affect the seizure threshold
Seizure risk associated with neuroactive drugs: Data from the WHO adverse drug reactions database; Kumlien E, Lundberg PO; Seizure (Dec 2009)
PURPOSE: To explore the association between the use of neuroactive drugs and reports of epileptic seizures. MATERIAL: Using the WHO adverse drug reactions (ADR) database, VigiBase, we surveyed reports of suspected seizures from 1968 until February 2006. Case reports of ADRs, that were classified as convulsions were collected and compared to the total number of ADRs reported. RESULTS: The total number of ADRs was 7,375,325. The number of convulsive events was 71,471. The ratio of convulsive ADRs to the total number of ADRs reported for each drug was evaluated and expressed as a percentage. The 10 drugs most frequently associated with convulsive ADRs were maprotilene (14.42%), escitaloprame (9.78%), buproprione (9.49%), clozapine (9.0%), chlorprothiexene (8.89%), amoxapine (8.74%), donepezil (8.40%), rivastigmine (6.41%), quetiapine (5.90%) and trimipramine (5.69%). CONCLUSIONS: Based on the reports in VigiBase, ADR reports relating to antidepressants, antipsychotic and cholinomimetic drugs included seizures more often than other neuroactive drugs.
Epilepsy random pearls
SMA atrophy
Human diseases with no mouse models
Treatment of Parkinson's disease: gyrokinetics
Sunday, August 02, 2009
tongue biting and seizures pearls
Lateral tongue biting is poorly sensitive but highly specific (99%) for a generalized seizure.
Lateral tongue biting usually indicates true epileptic seizures as opposed to bites to the tip of the tongue which are typically nonepileptiform events.
Lateral tongue biting has a predictive value of 71% for ipsilateral seizure focus.
from AAN website
Sunday, June 07, 2009
Differential diagnosis of thunderclap headache
Subarachnoid hemorrhage
unruptured aneurysm
cerebral sinus thrombosis
cervical artery dissection
hypertensive crisis
spontaneous intracranial hypotension
acute ischemic stroke
acute cerebral hematoma
pituitary apoplexy
intracranial infection
"benign" thunderclap (explode category)
Saturday, June 06, 2009
Treatable autoimmune encephalitis
17 patients were studied at University of Pennsylvania, as well as 22 "outside cases" with sera sent in. . The most important points were that
1. Most of the patients were accurately diagnosed clinically before antibodies were returned.
2. 9/17 had antibodies to known neuronal antigens (paraneoplastic or VGKC's) and 5/17 to novel cell membrane antigens (hippocampus/cerebellum). For the whole group, including the sent in cases, the numbers were 19/39 had antibodies to known antigens, 17/39 to nCMA's.
3. A significant treatment response effect was seen in those with VGKCA's and nCMA's.
4. Those with known intraneuronal antigens (anti Hu, anti Ma) are associated with cancer and may be associated with a worse prognosis than the antibodies to VGKCA's and nCMA's
5. Ovarian teratoma and thymoma are paraneoplastic treatable and benign conditions once the tumor is excised
6. No MRI or CSF characteristics help in diagnostic process.
In another article, some cases of ovarian teratoma associated paraneoplastic encephalitis are related to NMDA receptor antibodies (NMDAR) (Dalmau J, et al. Ann Neurol 2007; 61: 25-36. ) Posner's group described 12/12 with teratomas of ovary who had NMDAR with antibodies to the NR2 subunit, which binds glutamate in the forebrain and hippocampus, AND, a VIRUS LIKE PRODROME.
In yet another article, Mathew et al. (Neurology 2007; 68: 900-905) described orchiectomy for Ma2 related encephalitis as successful in showing otherwise undocumented tumors in 6/25 patients who underwent the procedure (the other 19 had known germ cell tumors). The criteria for orchiectomy were 1) present Ma2 antibodies with clinical/MRI evidence of encephalitis 2) life threatening or progressive neurologic deficits 3) age< 50 4) absent evidence for other tumors 5) new testicular enlargement, microcalcifications on testicular ultrasound, cryptorchidism or other evidence of testicular disease. All testicular specimens showed germ cell tumors. Tumor markers, body CT, PET, and other tests were negative in those undergoing the procedure.
Other antibodies reported include Hu, Ri, Ma1, Ma2, CAR, CRMP 3, amphiphysin, and others.
Thunderclap headache and benign CNS angiopathy
Chen SP et al. Reccurrent primary thunderclap headache and benign CNS angiopathy: spectra of the same disorder? Neurology 2006; 67:2164-2169.
56 patients with recurrent thunderclap headache were recruited. Segmental vasoconstriction was found in 22 (39 %). HA recurred .7 times per day for fourteen days. Each attack lasted 3 hours, and 84 % of patients reported at least one trigger. Nimodipine aborted attacks in 83 % and stopped headaches within 3 months. 4 patients (7%) developed stroke. Authors note that this entity is identical to benign CNS angiopathy. Exertion and defecation are greater triggers in vasoconstriction group. Other triggers are emotional situations,laughing, bathing, bending down.
Blogger note: this is identical to Call Fleming syndrome frequently discussed in USA. See http://strokenotes.blogspot.com/search?q=call for more minutiae about it.
Review article
Ducros A. Reversible cerebral vasoconstriction syndrome. Lancet Neurology 2012;11:906-917
additional pearls
1. Pain peaks in 1-2 weaks, angiogram findings in about 3 weeks.
2. Many synonyms exist (see below)
3. Thunderclap headache usually peaks within 1 minute, unilateral or bilateral and mimics aneurysm rupture; each episode may last 3 hours but can vary with up to 3 day duration, and 4 attacks over the 3 month period with moderate headache in between
4. Ten percent have focal findings; ten percent may have seizures including inaugural, and they rarely recur. Marching numbness can mimic migraine, focality, a stroke.
5. Beware of neck pain (dissection). Other differentials are CVT (check d Dimer and MRV), transfusion or products (red cell transfusion, alpha interferon, IVIG), phenytoin intoxication, CEA, low pressure headache.
6. May screen for pheochromocytoma or glomus tumor or carcinoid. Do a drug screen in some patients. Not only is cocaine in differential, cannabis is a trigger as well as LSD. Other triggers include SSRI's, triptans, ergot derivatives, nicotine patches, ginseng and binge drinking. Inquire about scorpion poison and star fruit.
7. Convexity SAH may be subtle, and missed on CT, strokes occur in watershed areas (including cerebellar watershed areas); brain edema can mimic PRES.
8. Catheter angiography can trigger TIA.
9. Postpartum cases occurs in first week after delivery. Inquire about exposure to vasoconstrictors during anesthesia, depression.
10. Synonyms and old names: isolated benign CNS vasculitis, acute benign cerebral angiopathy, reversible cerebral segmental vasoconstriction, Call Fleming syndrome, CNS pseudovasculitis, benign angiopathy of CNS, postpartum angiopathy, migraine angiopathy, migraine angiitis, migraine vasospasm, primary thunderclap headache, cerebral vasculopathy, vasospasm infatal migrainous infarction
11. Factors that independently make RCVS worse: those who receive glucocorticoids, serotonergic antidepressants, patients with ischemic stroke (Singhal AB, Topcuoglu MA. Glucocorticoid associated worsening in reversible cerebral vasoconstriction syndrome. Neurology 2017; 88:228-236.
Transient epileptic amnesia syndrome
Butler CR, Ann Neurol 2007; 61:587-598
Another hard to diagnose syndrome. 50 patients were recruited with recurrent amnesia, other cognitive functions intact, and compelling evidence of epilepsy. 24 controls also were studied. Clinical pearls to diagnosing this include: average age 62, frequent spells (eg one a month for a year), duration 30-60 minutes, occurrence upon awakening, prompt cessation with antiepileptic drug treatment. Neurocognitively patients complained of forgetting, but did well on standard (? what) neuropsych, but with accelerated forgetting of verbal and visual material over 3 weeks and some loss of autobiographical memory. Its diagnosis is usually missed.
Ictal asystole: clinical characteristics & SUDEP
Occurred in .27 % of patients undergoing VEEG. There was a sudden loss of atonia 42 seconds into the seizure with characteristic EEG findings of hypoperfusion. It occurred in TLE and extratemporal epilepsy. Clinical predisposing characteristics were not identified. Patients should be sent for pacemakers to avoid SUDEP.
Other predisposing factors for SUDEP are long QT syndrome, Brugada syndrome, and catecholaminergic ventricular arrythmia. Absence of treatment or insufficient treatment are neurologic risk factors.
Carbamazepine, which can decrease heart rate variability, has been proposed as a risk factor for SUDEP. SUDEP in most cases is triggered by a GTCS. Four cases that were monitored during SUDEP showed EEG flattening before cardiorespiratory changes. Another showed seizure triggered ventricular fibrillation. Sleeping prone may be a risk factor,
Nice review article:
Tomson T, Nashef L, Ryvlin P. Sudden unexpected death in epilepsy: current knowledge and future directions. Lancet Neurology 2008; 7:1021-1031.
More pearls Kloster R. et al. JNNP 1999; 67:439-444
risk factors
male predominance
Laying prone (17/24) usually during sleep.
At least one AED is subtherapeutic
Pulmonary edema is present in 26/42
Seizure just before death in 28/39
Alcohol levels were usually zero.
Friday, June 05, 2009
NeuroBehcet's pearls
multiple sources but NEJM CPC from May 28, 2009 was one.
1. Known as Silk Route disease due to occurrence along trading paths in Asia
2. Criteria include (major) oral ulcers occurring at least three times per year, genital ulcers or scars, ocular involvement (uveitis), skin (erythema nodosa, folliculitis, acne), positive skin pathergy test. Minor criteria are arthritis, DVT, superficial thrombophlebitis, epididymitis, positive family history, GI, CNS, or vascular involvement.
3. Neurologic involvement occurs in 5-10 %, with vascular involvement (venous sinus thrombosis or arterial thrombosis), or parenchymal infiltration. Brain stem and basal ganglia are common areas of predilection. The disease can be relapsing-remitting, chronic progressive, or secondary progressive.
4. Abnormal labs include high sed rate, CRP, complement, IL6,8 , TNF, and distinctive CSF neutrophilic pleocytosis.
5. Best treatment is not know, but in CPC authors suggested high dose pulsed steroid and cyclophosphamide, and maintenance immunoosuppression with azathioprine.
GAD 65 autoimmunity in PSP mimics
Article with reply by Mayo group in Neurology 1009 June. Original case was a 54 year old woman with supranuclear gaze plasy and parkinsonism mimicking PSP. There were stiff man like symptoms and strong GAD65 positivity. PSP was excluded in part by prominent early upgaze palsy, and startle induced spasms typical of SMS, and video ENG findings of a fatiguing pattern of saccade initiation with repetive saccades. The Mayo report (Pittock SJ, Mayo Clin Proc 2006) presented with brainstem, eps and spinal cord syndromes and were initially misdiagnosed as PSP or MSA. Pittock's group also reported OCB in CSF and improvement with prompt initiation of immunotherapy.
Superior division oculomotor paresis
Clin note in Neurology June 2009.
KEY POINTS
Clinical Patient has diplopia in vertical gaze, right ptosis, and right retroorbital pain. Exam showed ptosis, hypotropia, and elevation paresis in the right eye (looking in and up). Angio showed cavernous right ICA aneurysm that was coiled. The IIIn divides into superior and inferior divisions near SOF or anterior cavernous sinus. Clinical presentation is ptosis and superior rectus palsy.
Monday, May 11, 2009
BNP levels in neurologic disease
2 uses
1. Document cadiac valvulopathy among patients exposed to pergolide
2. Document CHF in stroke patients ie possible need for anticoagulation and cardiac evaluation
SWEDDs non Parkinson's disease
4-15 % of patients entered into trials for PD had normal presynaptic nigrostriatal dopaminergic imaging and were termed "subjects with scans without evidence of dopaminergic deficits." (SWEDD's). Withdrawal of dopamine was nondeleterious and rescanning 4 years later continued to show no deficit. Case was presented of a subject with jerky assymmetric rest and action tremor, arm dystonia, hypomimia, increased limb tone, and slow repetitive finger movements. 3/10 had abnormal thumb extension (Froment's sign in this case), none had micrographia, and none had loss of sense of smell. True bradykinesia, as defined by progressive decrement of speed and amplitude of repetitive movement (decremental bradykinesia) was not present and should be contrasted to just slowing or hesitation of voluntary movement. The action tremor occurred as the arms were held up (postural tremor).
Blogger note: differential diagnosis could include corticobasal ganglionic degeneration, difference being more rapid progression in that condition, particularly if functional imaging is not done or not available.
Small, spastic furrowed tongue of Allgrove's syndrome
Houlden H. Neurology (Neuroimages) 2009; 72:1366.
35 yo with slowly progressive achalasia, alacrima, motor neuropathy, bulbar palsy, and a small furrowed tongue. Sister had same plus adrenal deficiency (triple A syndrome). DNA analysis of ALADIN gene confirmed.
Chronic progressive myeloneuropathies
Nutritional deficiency-- B12, folate, vitamin E, copper, nitrous oxide deficiency with impaired
B12 metabolism, AIDS myelopathy with impaired B12 metabolism
Infectious-- HTLV I, AIDS, syphilis
Inflammatory- Sjogren's, sarcoid
Geographic - toxic-- cassova toxicity, lathyrism, fluorosis, subacute optico myeloneuropathy,
tropical myeloneuropathies
Toxic-- chemo ( cisplatin, cytarabine, intrathecal therapy, organophosphate
Genetic
With metabolic abnormality: adrenomyeloneuropathy, Krabbe disease, MLD, CTX, familial
vitamin E deficiency, abetalipoproteinemia, cobalamin and foalte metabolism defects,
respiratory chain defects, APBD
Without metabolic abnormalities: HSP, SCA
Evaluation:
vitamin B12, folate, vitamin E, calcium, glucose, TSH, alkphos, lactate, pyruvate, paraneoplastic screen, arylsulfatase A, beta galactosidase, peroxisomal screen ( VLCFA, pristanic acid, phytanic acid), ACE level, ceruloplasmin, copper, ANA, cyclic citrullinated peptide antibodies, SPEP, SIEP, lyme screen, VDRL, HIV, HTLV I/II, NMO IgG, SSA, antibodies to Gad 65, AST, ALT
CSF--cells, diff, MS panel, lyme titers, JC virus pcr, and paraneoplastic screen.
APBD Adult polyglucosan body disease
Neurology 2009; 72: 1609-1613 (CPC)
Jewish diseases with leukoencephalopathy:
APBD--Ashkenazi
megelencephalic encephalopathy with subcortical cysts-- Libyan
mitochondrial neurogastrointestinal encephalomyelopathy-- Ashkenazi and Libyan
cerebrotendinous xanthomatosis-- Moroccan
metachromatic leukodystrophy-- Yemenite
Canavan disease
mucolipidosis type IV
APBD-- uniquely occurs in 50 yo with CNS and PNS involvement
AR
diagnosis with skin.fibroblasts measurement of glycogen branching enzyme activity
Genetic spectrum well beyond Ashkenazi Jews. Allelic to type 4 glycogen storage disease. Unlike glycogen storage, liver is affected in kids.
Clinical
progressive late onset spastic paraparesis, progressive, neurogenic bladder, sensorimotor neuropathy with painful feet. Cognitive involvement even dementia is common.
CSF normal
MRI progressive involvement of hemisphere and PVWM, post limb of ic, brainstem tracts, sparing of corpus callosum and u fibers. Lesions are hyperintense on T2 and not enhancing. Atrophy of spinal cord is early and invariable. Sural nerve biopsy or axillary apocrine biopsy are diagnostic of polyglucosan bodies.
Monday, March 16, 2009
UPDRS
Hoehn and Yahr Staging of Parkinson's Disease
1. Stage One
1. Signs and symptoms on one side only
2. Symptoms mild
3. Symptoms inconvenient but not disabling
4. Usually presents with tremor of one limb
5. Friends have noticed changes in posture, locomotion and facial expression
2. Stage Two
1. Symptoms are bilateral
2. Minimal disability
3. Posture and gait affected
3. Stage Three
1. Significant slowing of body movements
2. Early impairment of equilibrium on walking or standing
3. Generalized dysfunction that is moderately severe
4. Stage Four
1. Severe symptoms
2. Can still walk to a limited extent
3. Rigidity and bradykinesia
4. No longer able to live alone
5. Tremor may be less than earlier stages
5. Stage Five
1. Cachectic stage
2. Invalidism complete
3. Cannot stand or walk
4. Requires constant nursing care
This rating system has been largely supplanted by the Unified Parkinson's Disease Rating Scale, which is much more complicated.
Unified Parkinson's Disease Rating Scale (UPDRS)
The UPDRS is a rating tool to follow the longitudinal course of Parkinson's Disease. It is made up of the 1) Mentation, Behavior, and Mood, 2) ADL and 3) Motor sections. These are evaluated by interview. Some sections require multiple grades assigned to each extremity. A total of 199 points are possible. 199 represents the worst (total) disability), 0--no disability.
I. Mentation, Behavior, Mood
Intellectual Impairment
0-none
1-mild (consistent forgetfulness with partial recollection of events with no other difficulties)
2-moderate memory loss with disorientation and moderate difficulty handling complex problems
3-severe memory loss with disorientation to time and often place, severe impairment with problems
4-severe memory loss with orientation only to person, unable to make judgments or solve problems
Thought Disorder
0-none
1-vivid dreaming
2-"benign" hallucination with insight retained
3-occasional to frequent hallucination or delusions without insight, could interfere with daily activities
4-persistent hallucination, delusions, or florid psychosis.
Depression
0-not present
1-periods of sadness or guilt greater than normal, never sustained for more than a few days or a week
2-sustained depression for >1 week
3-vegetative symptoms (insomnia, anorexia, abulia, weight loss)
4-vegetative symptoms with suicidality
Motivation/Initiative
0-normal
1-less of assertive, more passive
2-loss of initiative or disinterest in elective activities
3-loss of initiative or disinterest in day to say (routine) activities
4-withdrawn, complete loss of motivation
II. Activities of Daily Living
Speech
0-normal
1-mildly affected, no difficulty being understood
2-moderately affected, may be asked to repeat
3-severely affected, frequently asked to repeat
4-unintelligible most of time
Salivation
0-normal
1-slight but noticeable increase, may have nighttime drooling
2-moderately excessive saliva, hay minimal drooling
3-marked drooling
Swallowing
0-normal
1-rare choking
2-occasional choking
3-requires soft food
4-requires NG tube or G-tube
Handwriting
0-normal
1-slightly small or slow
2-all words small but legible
3-severely affected, not all words legible
4-majority illegible
Cutting Food/Handing Utensils
0-normal
1-somewhat slow and clumsy but no help needed
2-can cut most foods, some help needed
3-food must be cut, but can feed self
4-needs to be fed
Dressing
0-normal
1-somewhat slow, no help needed
2-occasional help with buttons or arms in sleeves
3-considerable help required but can do something alone
4-helpless
Hygiene
0-normal
1-somewhat slow but no help needed
2-needs help with shower or bath or very slow in hygienic care
3-requires assistance for washing, brushing teeth, going to bathroom
4-helpless
Turning in Bed/ Adjusting Bed Clothes
0-normal
1-somewhat slow no help needed
2-can turn alone or adjust sheets but with great difficulty
3-san initiate but not turn or adjust alone
4-helpless
Falling-Unrelated to Freezing
0-none
1-rare falls
2-occasional, less than one per day
3-average of once per day
4->1 per day
Freezing When Walking
0-normal
1-rare, may have start hesitation
2-occasional falls from freezing
3-frequent freezing, occasional falls
4-frequent falls from freezing
Walking
0-normal
1-mild difficulty, day drag legs or decrease arm swing
2-moderate difficultly requires no assist
3-severe disturbance requires assistance
4-cannot walk at all even with assist
Tremor
0-absent
1-slight and infrequent, not bothersome to patient
2-moderate, bothersome to patient
3-severe, interfere with many activities
4-marked, interferes with many activities
Sensory Complaints Related to Parkinsonism
0-none
1-occasionally has numbness, tingling, and mild aching
2-frequent, but not distressing
3-frequent painful sensation
4-excruciating pain
III. Motor Exam
Speech
0-normal
1-slight loss of expression, diction,volume
2-monotone, slurred but understandable, mod. impaired
3-marked impairment, difficult to understand
4-unintelligible
Facial Expression
0-Normal
1-slight hypomymia, could be poker face
2-slight but definite abnormal diminution in expression
3-mod. hypomimia, lips parted some of time
4-masked or fixed face, lips parted 1/4 of inch or more with complete loss of expression
*Tremor at Rest
Face
0-absent
1-slight and infrequent
2-mild and present most of time
3-moderate and present most of time
4-marked and present most of time
Right Upper Extremity (RUE)
0-absent
1-slight and infrequent
2-mild and present most of time
3-moderate and present most of time
4-marked and present most of time
LUE
0-absent
1-slight and infrequent
2-mild and present most of time
3-moderate and present most of time
4-marked and present most of time
RLE
0-absent
1-slight and infrequent
2-mild and present most of time
3-moderate and present most of time
4-marked and present most of time
LLE
0-absent
1-slight and infrequent
2-mild and present most of time
3-moderate and present most of time
4-marked and present most of time
*Action or Postural Tremor
RUE
0-absent
1-slight, present with action
2-moderate, present with action
3-moderate present with action and posture holding
4-marked, interferes with feeding
LUE
0-absent
1-slight, present with action
2-moderate, present with action
3-moderate present with action and posture holding
4-marked, interferes with feeding
*Rigidity
Neck
0-absent
1-slight or only with activation
2-mild/moderate
3-marked, full range of motion
4-severe
RUE
0-absent
1-slight or only with activation
2-mild/moderate
3-marked, full range of motion
4-severe
LUE
0-absent
1-slight or only with activation
2-mild/moderate
3-marked, full range of motion
4-severe
RLE
0-absent
1-slight or only with activation
2-mild/moderate
3-marked, full range of motion
4-severe
LLE
0-absent
1-slight or only with activation
2-mild/moderate
3-marked, full range of motion
4-severe
*Finger taps
Right
0-normal
1-mild slowing, and/or reduction in amp.
2-moderate impaired. Definite and early fatiguing, may have occasional arrests
3-severely impaired. Frequent hesitations and arrests.
4-can barely perform
Left
0-normal
1-mild slowing, and/or reduction in amp.
2-moderate impaired. Definite and early fatiguing, may have occasional arrests
3-severely impaired. Frequent hesitations and arrests.
4-can barely perform
*Hand Movements (open and close hands in rapid succession)
Right
0-normal
1-mild slowing, and/or reduction in amp.
2-moderate impaired. Definite and early fatiguing, may have occasional arrests
3-severely impaired. Frequent hesitations and arrests.
4-can barely perform
Left
0-normal
1-mild slowing, and/or reduction in amp.
2-moderate impaired. Definite and early fatiguing, may have occasional arrests
3-severely impaired. Frequent hesitations and arrests.
4-can barely perform
*Rapid Alternating Movements (pronate and supinate hands)
Right
0-normal
1-mild slowing, and/or reduction in amp.
2-moderate impaired. Definite and early fatiguing, may have occasional arrests
3-severely impaired. Frequent hesitations and arrests.
4-can barely perform
Left
0-normal
1-mild slowing, and/or reduction in amp.
2-moderate impaired. Definite and early fatiguing, may have occasional arrests
3-severely impaired. Frequent hesitations and arrests.
4-can barely perform
*Leg Agility (tap heel on ground, amp should be 3 inches)
Right
0-normal
1-mild slowing, and/or reduction in amp.
2-moderate impaired. Definite and early fatiguing, may have occasional arrests
3-severely impaired. Frequent hesitations and arrests.
4-can barely perform
Left
0-normal
1-mild slowing, and/or reduction in amp.
2-moderate impaired. Definite and early fatiguing, may have occasional arrests
3-severely impaired. Frequent hesitations and arrests.
4-can barely perform
*Arising From Chair (pt. arises with arms folded across chest)
0-normal
1-slow, may need more than one attempt
2-pushes self up from arms or seat
3-tends to fall back, may need multiple tries but can arise without assistance
4-unable to arise without help
*Posture
0-normal erect
1-slightly stooped, could be normal for older person
2-definitely abnormal, mod. stooped, may lean to one side
3-severely stooped with kyphosis
4-marked flexion with extreme abnormality of posture
*Gait
0-normal
1-walks slowly, may shuffle with short steps, no festination or propulsion
2-walks with difficulty, little or no assistance, some festination, short steps or propulsion
3-severe disturbance, frequent assistance
4-cannot walk
*Postural Stability (retropulsion test)
0-normal
1-recovers unaided
2-would fall if not caught
3-falls spontaneously
4-unable to stand
*Body Bradykinesia/ Hypokinesia
0-none
1-minimal slowness, could be normal, deliberate character
2-mild slowness and poverty of movement, definitely abnormal, or dec. amp. of movement
3-moderate slowness, poverty, or small amplitude
4-marked slowness, poverty, or amplitude
Schwab and England Activities of Daily Living
Gillingham FJ, Donaldson MC, eds., Third Symp. of Parkinson's Disease, Edinburgh, Scotland, E&S Livingstone, 1969, pp.152-7.
Rating can be assigned by rater or by patient.
* 100%-Completely independent. Able to do all chores w/o slowness, difficulty, or impairment.
* 90%-Completely independent. Able to do all chores with some slowness, difficulty, or impairment. May take twice as long.
* 80%-Independent in most chores. Takes twice as long. Conscious of difficulty and slowing
* 70%-Not completely independent. More difficulty with chores. 3 to 4X along on chores for some. May take large part of day for chores.
* 60%-Some dependency. Can do most chores, but very slowly and with much effort. Errors, some impossible
* 50%-More dependant. Help with 1/2 of chores. Difficulty with everything
* 40%-Very dependant. Can assist with all chores but few alone
* 30%-With effort, now and then does a few chores alone of begins alone. Much help needed
* 20%-Nothing alone. Can do some slight help with some chores. Severe invalid
* 10%-Totally dependant, helpless
* 0%-Vegetative functions such as swallowing, bladder and bowel function are not functioning. Bedridden.
Disclaimer: The information and reference materials contained herein is intended solely for the information of the reader. It should not be used for treatment purposes, but rather for discussion with the patient's own physician.
A Good Credit Score is 700 or Above. See yours in just 2 easy steps!